Prescription of Antibiotics in Dentistry?
As dentists prescribe approximately 10% of antibiotics dispensed in primary care, it is important not to underestimate the potential contribution of the dental profession to the development of antibiotic resistant bacteria.
Antibiotics do not reduce pain or swelling arising from teeth with symptomatic apical pathosis in the absence of evidence of systemic involvement. Infection must be systemic or the patient must be febrile or immunocompromised to justify the need for antibiotics. For these reasons, prescription of antibiotics by dentists should be limited.
Empirical prescription
In dentistry, antibiotic prescription is empirical because the dentist does not know what microorganisms are responsible for the infection.
Inappropriate use of antibiotics not only drives antibiotic resistance and misuses resources but also increases the risk of potentially fatal anaphylactic reactions and exposes people to unnecessary side effects.
In addition, antibiotic prescribing for common medical problems increases patient expectations for antibiotics, leading to a vicious cycle of increased prescribing in order to meet expectations.
Thus, microorganisms responsible for the infections can only be suspected, and treatment is decided on a presumptive basis with broad-spectrum antibiotics often being prescribed.
Systemic versus topical use of antibiotics in Endodontic treatments
Systemic antibiotics should be used in: localized fluctuant swellings, patient with systemic disease causing impaired immunologic function, elevated body temperature (>38 °C), lymphadenopathy, osteomyelitis…etc. Also, in the treatment of traumatic injuries of the teeth such as luxation injuries of the permanent dentition, replantation of avulsed teeth.
On the other hand, use of topical antibiotics has been proposed for several endodontic treatments: pulp capping, root canal treatment, regenerative endodontic procedures, tooth avulsion.

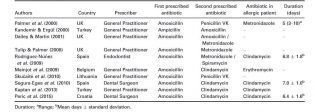
Which antibiotic and for how long?
Amoxicillin is the preferred antibiotic in endodontic infections either used alone or in combination with clavulanic acid. It is a moderate-spectrum, bacteriolytic, β-lactam antibiotic that represents a synthetic improvement upon the original penicillin molecule.
It is good for oral facial infection because it is readily and better absorbed than penicillin and can be taken with food.It has better ability to resist damage from stomach acid so less oral dose is wasted and a much broader spectrum against gram-negative cell wall than penicillin. Due to its longer half-life and more sustained serum levels, it only requires administration three times a day and costs only slightly more than penicillin.
The general tendency to administer an antibiotic is 3-7 days. Prolonged antibiotic usage will destroy the commensal flora in the oral cavity and other terminates colonization resistance.
Summarizing…
Odontogenic infections are polymicrobial in nature. Prompt diagnosis and treatment, including elimination of the causative factor, are crucial to their successful management. Antibiotics are a useful adjunct in the treatment of odontogenic infections, but should not replace removal of the causative factor. All dentists and any other specialists should be aware of the correct usage of antibiotics.
This post was written by King Shuen Judy Yim, Tzu-Han Lin, Hsun-Wen Liu, Marie-Amélie Saugues, and Yun-Yun Yu, 2nd Year Dentistry Students in Microbiology and Virology, well done!
References
https://onlinelibrary.wiley.com/doi/epdf/10.1111/iej.12741
https://jcda.ca/article/a37
https://hal.univ-lorraine.fr/hal-01931879/document












