Remember what I told you last week? Every Wednesday we talk about health. This session was about palliative care, dedicated to nursing students. Hold on because that was my thought before listening to the doctors; in reality, it´s an important field that not many professionals ever think about when they are studying in universities. We were happy to have Dr Begoña Reig Molla, a family doctor and an associated teacher of General Pathology in CEU Valencia to explain to us how the system works. Moreover, Dr Emilio García Sánchez from the University of Navarra gave a talk about ethical questions in palliative care for people on their last day of life.
Why is palliative care important?
The term is coined by Dame Cicely Saunders, the founder of St Christopher’s Hospice in London and she was a nurse. It’s defined as a way of caring for people with life-threatening illnesses physically and mentally. The comfort of the patient in physical, emotional, spiritual & social aspect are the main objectives of it. We always have to avoid saying ‘we cannot do anything for the patient’; at the same time promote the dignity of the sicker. Besides, the patient’s family is also considered as a fundamental criterion to support the patient through this hard time.
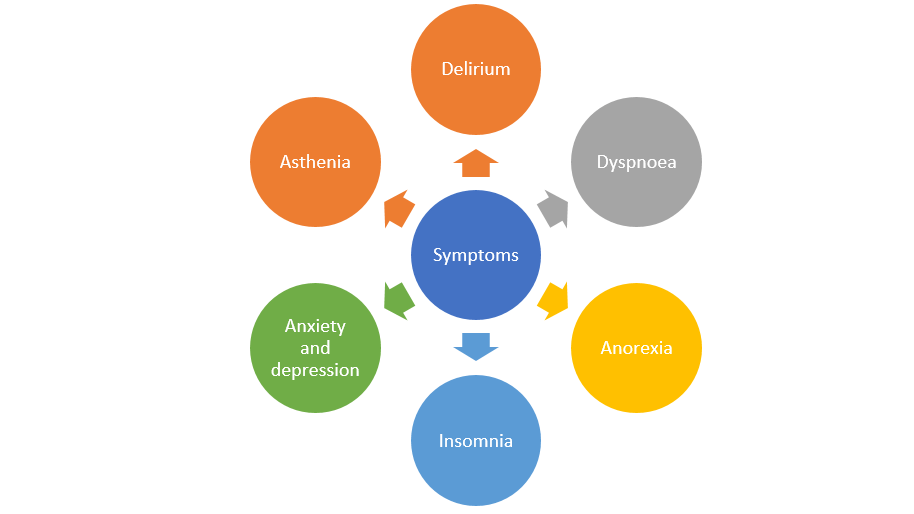
A basic guidance is composed, in which the symptoms control process is very important: it can be with or without medicine, but the goal is a total analgesic.
Nevertheless, we count on nursing care, which consists of:
- Take care of the skin: maintain good hygiene, prevent ulcers, inflammations, infections and be careful in changing patient position.
- Avoid injuries in the face, especially buccal part.
- Take care of environmental effects, such as sleep, food, rooms, family members…
Dr Reig is a member of EAP (Equipo de Atención Primaria – Team of Primary Care) in Valencia and she has been working with many cases and families.
Ethical concern regarding palliative care
Mr Emilio García had to remind us how modern technologies have evolved in order not to accelerate the crazy actions of pain in these severe diseases. The company of health carers to a patient till the end of his/her lifetime is a brave effort because it’s not easy facing the death in front of your eyes. This is the art I was talking about: when there is no way to cure the disease, make the patient want to keep living, hold up the hope and motivation in life and feel the patient’s value. Even you are not succeeded, do not let the patient think about the bad thing; in another word, do not let them sense the pain.
There were two real stories that the two doctors wanted to tell us. The first one was a Muslim patient in hospital La Fe in Valencia, that he could not calm down in his last days of life, eventhough many measures had been taken; until a prophet came to his room in the hospital and gave a talk for 30 minutes. The next story was told by a colleague of Dr García in London, who had been working in palliative care for 25 years, and she could not forget this military man. During his time in the hospital, she came an hour every day to talk with him, and for 3 months he always asked for a pill to die. She felt very strange and told him:
– Why do you want to die when we have had a good time talking together?
-Because after you left, I was alone again and I have to wait 23 hours more till you make me smile – he responded.

I want to make the point here. People believe in different things and we can try to hit the target. Inject a painkilling drug to a patient is what any of health professional can, but to be a palliative doctor/nurse/pharmacist, it’s required more than finishing a degree.







