According to the WHO definition, adherence is ‘the extent to which a person’s behavior – taking medication, following a diet and/or executing lifestyle changes – corresponds with agreed recommendations from a healthcare provider’. From this definition, we can also understand the concept of non-adherence, which is the refusal to comply with some or all of the recommendations of our healthcare professionals. Non-adherence to treatment can lead to several consequences that are harmful to the patient and make the healthcare system less efficient. Regarding the consequences to the patient, the recovery from his condition can be less efficient, or worse, he can have undesirable effects from not taking his medication as prescribed. The main tools that healthcare professionals have to fight this include adequate verbal communication methods and a system for prescriptions and the medical history of the patient that is efficient.
Here are some examples of behaviors that we healthcare professionals can use to improve treatment adherence:
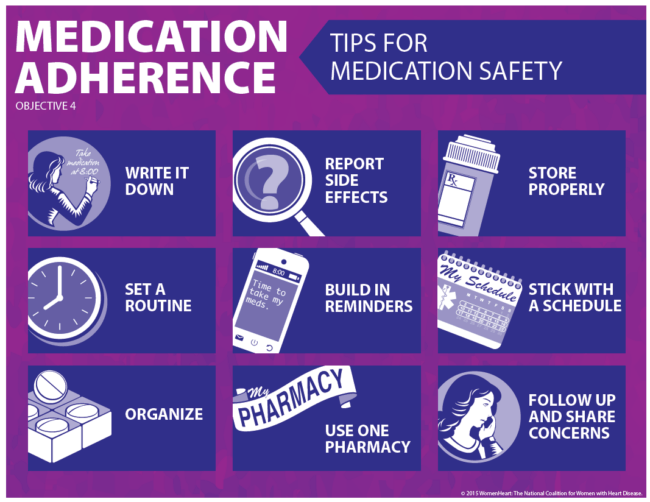
First, it is helpful and necessary for a health professional to get to know the sociocultural environment and the different beliefs that the patients may have. This is done by asking the right questions during the medical interview but also by observing the patient, his age, and appearance. One should never judge or criticize a patient for their choices, rather the information we gather should be used to adapt the treatment to them. We must respect the refusal to take the treatment and offer alternatives when possible. Furthermore, the health professional needs to give a detailed explanation of how to take the medication and the possible negative effects of not taking it as indicated. It is important to adapt the medical vocabulary to the patient. Use simple straightforward words and always make sure that they have understood before moving on. Since there is a risk that the patient forgets some of the indications, writing them down clearly on the prescription or a sheet of paper can make a huge difference. This is important especially in the elderly population as they often have multiple medications from multiple specialists. Moreover, it is important as much as possible to ask the patient about the difficulties he may have had with the treatment. It is crucial to carry this out in a non-judgmental or patronizing manner but always with respect and compassion. It is common for patients to feel guilt when they did not manage to comply with a certain treatment, rather than only explaining how harmful their lack of adherence is (they often already know it), it is more efficient to investigate what aspects of the treatment they have difficulties with. Sometimes it is because of a side effect that they wish to avoid or simply the fact that they forget to take it. Sometimes there is the option of changing the medication or posology but we can also assist the patient by teaching them tools to remember to take their medications such as alarms, mobile apps, pill boxes, or assistance from their close one.
Finally, doctors need to write clearly in the medical history of the patient the different issues they may have regarding adherence which will make it easier for other health professionals that treat the patient to adapt their communication methods to them. The more you write the better, even interactions that do not seem significant medically might give a lot of information on the patient and his personality. Writing also protects professionals from legal charges if the patient fails to follow through with the recommendations, so it is essential for both sides. We see overall that the relationship that the patient has with his doctor will greatly influence how they take their treatment. It is therefore essential to follow these recommendations but above all, to remain modest, understanding, and respectful when approaching them. Remember that our priority is not to be right, but to do what is right for the patient.
By Marina Figueredo & Luis D’Marco